MEMBER RESOURCES
We want to ensure that our participants always have a positive customer service experience.
Understanding how your Benefit Plan works and how to use it empowers you. Promoting your access to services to support your good health and well-being is in the forefront of all we do.
In furtherance, we do the following:
- Assist you with navigating your benefit plan maze – providing you with benefit information, eligibility and resources.
- Provide you with “one call issue resolution” to resolve any questions, problems or help you access providers.
- Empower you with the informational tools to be a wise consumer of your health benefits.

Current members:
- Find a doctor
- Check the status of a claim
- Replace a membership card
Member Benefits:
- Superior Customer Service
- Member Advocacy
- Care Coordination
- Quality & Cost Transparency
Our goal is to eliminate any stress and confusion from your benefits experience. We are here to help you if you have questions or have an issue. Our goal is to resolve issues with one phone call.
Where do I go from here?
If you are a member:
Call us at the number on the back of your card (800) 585-5965.
- Check eligibility and benefits
- Check claim status
- Obtain benefits
- Find an in-network provider
- Request copy of an EOB
If you are a provider:
Call us at the number on the back of your card (800) 585-5965.
- Obtain claim address and fax number
- Get an authorization for elective services
- Check claim status
- Check eligibility
- Secure patient coverage information
- Request a remittance advice
FIND A PROVIDER:
Understanding your EOB:
An Explanation of Benefits (EOB) is a document which provides the details of a processed claim. Our EOB clearly shows who was paid, how much was paid and if any additional payment is required by the participant. Remember to save your EOBs for tax purposes and as a record for treatment dates and services.
- Find a provider
- Understand my EOB
- Download forms
- Email a claim
Please contact Centrix via telephone or fax
Member Forms:
These forms are for our members to use in managing their benefit plans. The benefit plan forms posted here are general forms. Should you require assistance or have questions please do not hesitate to call: (800) 585-5965.
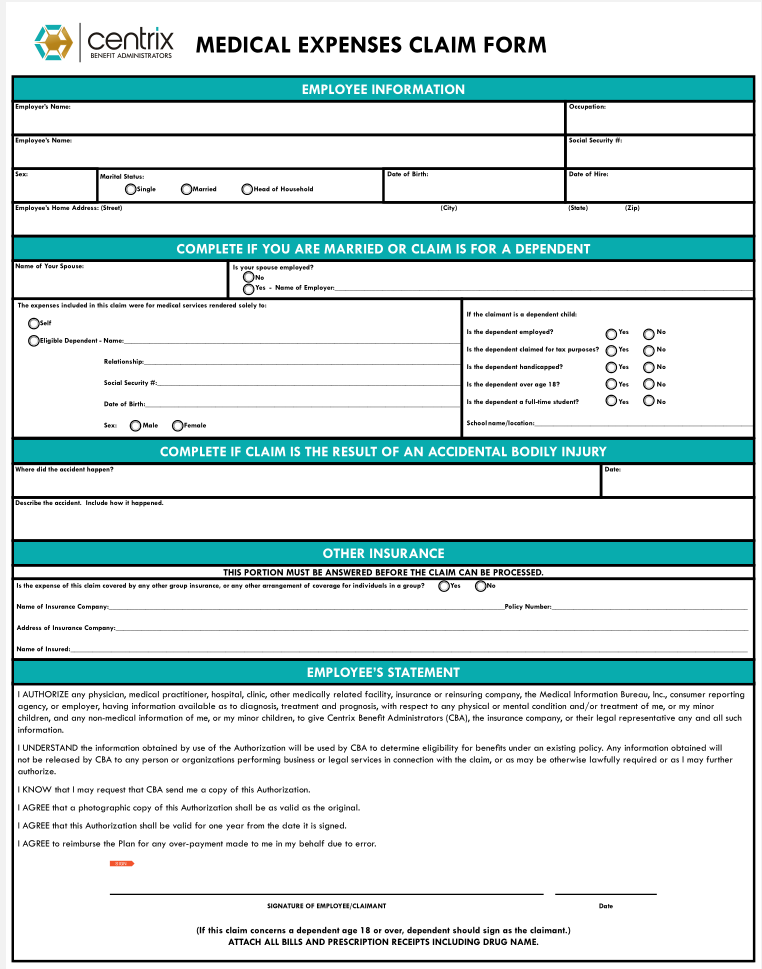
- Medical Claim Reimbursement Form
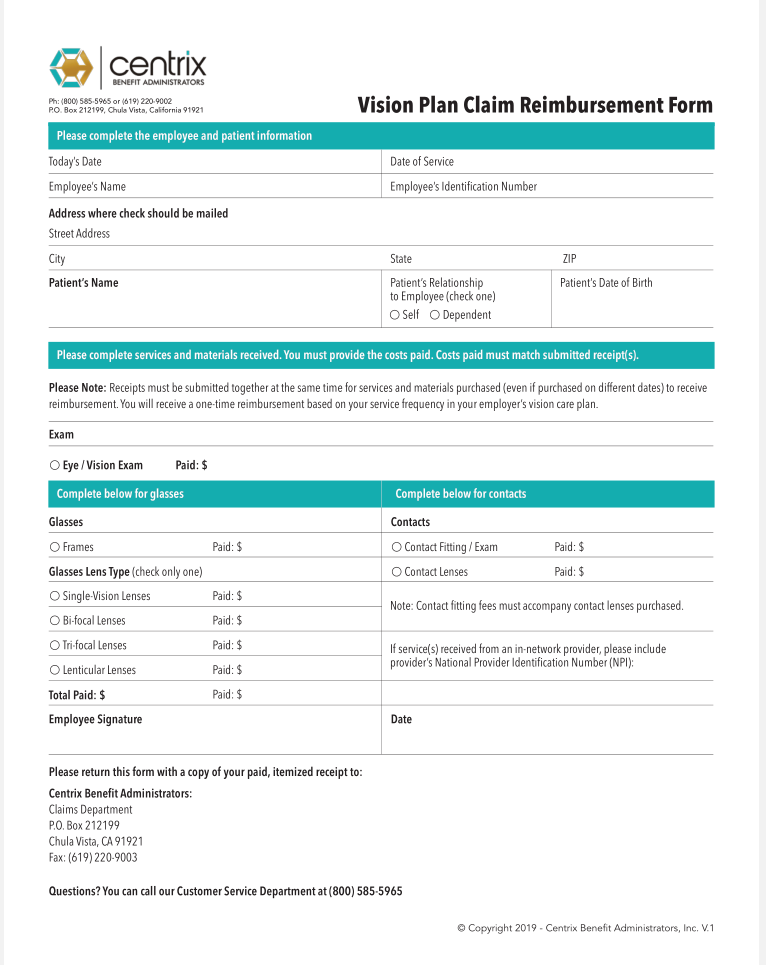
- Vision Claim Reimbursement Form
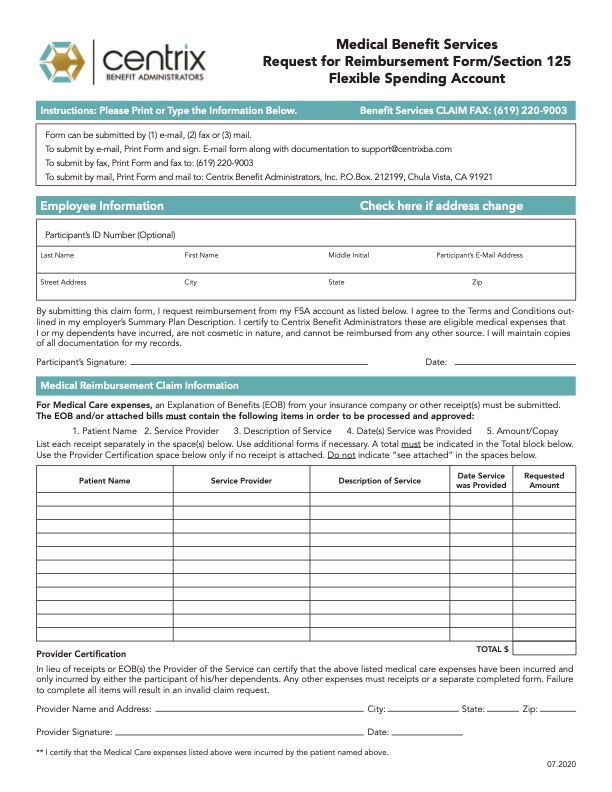
- FSA Claim Reimbursement Form
- Employee Enrollment Form
- SBC Uniform Glossary
Email a Claim:
Please note that only your actual scanned file will be reviewed. If you have any comments, instructions or important information that needs to be included with your claim, please be sure to include it in the scanned file. No reply will be sent after receipt of your claim. The contents of your claims file will be scanned and be entered into our normal claims processing flow. You will proceed to the e-mail screen where you will attach your scanned claims file after clicking the “I accept these conditions” button below.